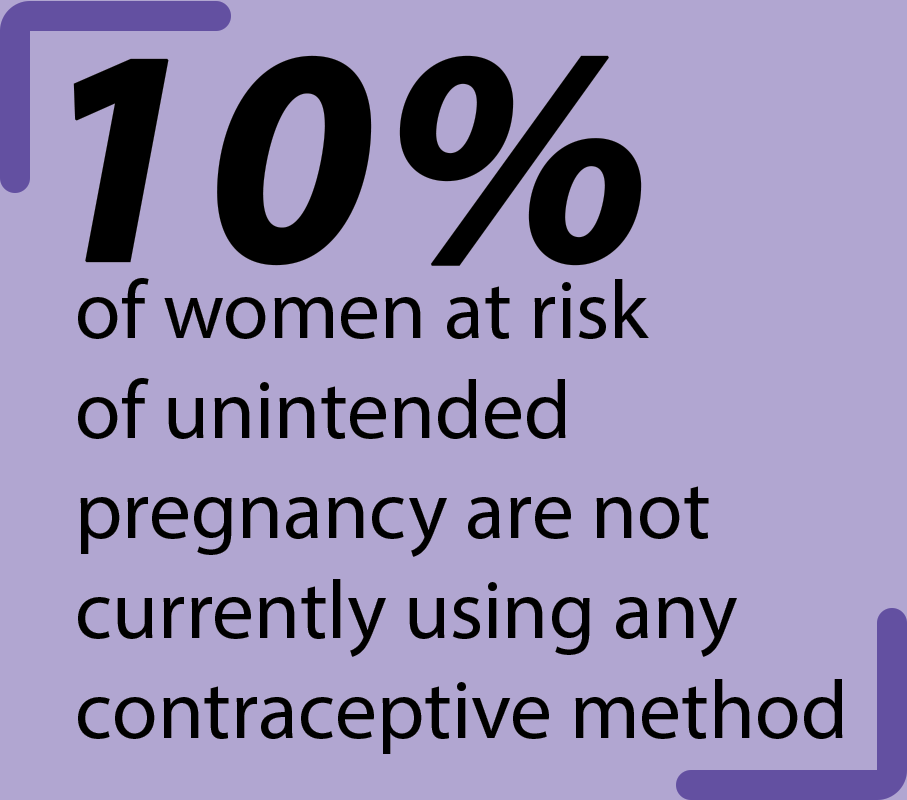
 While the school requires students to learn the basis of contraceptives, many remain ill-informed about the history and many uses of birth control. Birth control does play a large role in preventing unwanted pregnancies, but it is also used to address other health concerns.
While the school requires students to learn the basis of contraceptives, many remain ill-informed about the history and many uses of birth control. Birth control does play a large role in preventing unwanted pregnancies, but it is also used to address other health concerns.
The first form of a birth control pill was originally approved by the Food and Drug Administration for severe menstrual disorders and had an increased risk of breast cancer and endometrial cancer that was concerning for women, according to Planned Parenthood. It was not approved to prevent pregnancy until 1960.
According to Planned Parenthood, barrier methods, any contraceptive that is used to physically prevent sperm from reaching the egg, were originally made of natural materials, such as honey, crocodile dung and lead. The first tubal sterilization in the U.S. was performed in Toledo, Ohio in 1880, and vasectomies were exclusively used as a punishment for disabled or non-white males until the 1960s, when the women’s movement took off.
Male condoms have been used for centuries with only minor changes to the material, and female condoms were introduced in 1994, according to Planned Parenthood. The first version of an IUD was invented in Germany in 1909 and released in 1945, while the first implant was invented in 1995.
Clinical Research Specialist and Nurse Practitioner Kathryn Martin said that for a patient to be given a prescription form of birth control, they have to make an appointment with a gynecologist for an assessment of risk factors. Patients might already know what form of birth control they want, but doctors can make recommendations based on the health check and their previous work with certain types of contraceptives, she said.
The risk factors that doctors check are age, blood pressure, past conditions with heart problems or blood clotting, cancer, pregnancy, allergies and smoking, she explained.
Gynecologists are needed to prescribe Progestin IUD, copper IUD, implant, Depo-Provera shot, birth control pills, Progestin-Only pills, transdermal patch and vaginal ring in Ohio, she said. Martin added that male and female condoms, pulling out, diaphragms, cervical caps, fertility awareness, spermicide and emergency contraception pills are all options to patients without doctor involvement.
According to Planned Parenthood, a Progestin IUD is inserted into the uterus, an implant is inserted into the arm and a vaginal ring is inserted into the vagina to release hormones that prevent pregnancy. A copper IUD is also inserted into the uterus but does not release hormones. The shot, patch and pills all release hormones into the body. Diaphragms and cervical caps are both placed over the cervix to prevent sperm from entering, but they have different shapes.
Fertility awareness requires women to track their menstrual cycle to when their uterus releases an egg so that they can avoid having sex near ovulation, the 13-15 day period before the start of menstration when an egg is released from the ovary into the fallopian tube. Spermicide is a chemical substance put into the vagina to prevent the sperm from reaching the egg.
Martin added that during her time working in women’s health, most females between 15 and 35 choose the pill, and once they are done having children, they opt for a less user-dependent form of birth control, like an IUD. She said that most adolescent gynecology clinics try to steer teens away from choosing the pill because they are worried that they will forget to take the pill at the same time every day. However, once a person reaches menopause around 51, they no longer need birth control, she said.
“We just consider every woman up until 51 as being able to become pregnant, so we counsel all women up until that point that you need to think about using something for birth control,” Martin said.
Contraceptives can also be used to address irregular or painful periods, acne and recurrent ovarian cysts, she added.
Assistant Professor of General Obstetrics and Gynecology at The Ohio State University Megan Quimper said that condoms are the only form of contraceptive that protect against sexually transmitted diseases, along with getting regularly tested.
The most common STDs are gonorrhea, chlamydia, trichomoniasis and herpes, she explained. She said gonorrhea, chlamydia and trichomoniasis are bacterial diseases and can be treated with antibiotics, while herpes is a viral disease and has an antiviral medication to get rid of symptoms but can not be cured.
In the 45 years that Martin has been working in women’s health, she said that while she has seen advances in contraception devices and methods, she has not seen a significant change in the stigma surrounding birth control.
“I feel that birth control has come a long way,” Martin said. “We still have to think about the political and religious overtones that are still present in our country.”
She added that sexism around the topic is still very present.
“In our country, and it’s true in the entire world, it’s a responsibility that falls onto the woman,” Martin said. “Every day, they’re trying to develop a birth control pill for a male that a man can take, but to be honest with you, it’s just kind of a joke in a way that many people laugh at.”
Despite the skepticism, a male hormonal birth control pill is being developed along with an IUD that lasts for 10 years, she said. Current research is also aimed toward limiting the effects of current birth control pills and developing extended cycle pills, she added. Martin explained that the present birth control pill can be taken for three weeks straight, excluding a fourth week so the person can menstruate. An extended cycle pill would be taken for a longer period of time so that a person does not have their period once every month, and they can have a longer break in between, she added.
Martin said that a development throughout her time working with contraceptives is that people are more open to talking about women’s health regarding birth control.
“At least for me, in my age, being in high school 40 years ago, we did not talk about how to prevent pregnancy,” Martin said. “We just talked about how it happens, but then the conversation stopped there, and you just didn’t have a baby until you were ready to have a baby. Fortunately, that has changed.”